Expert Perspective: The Case for Patient Access Medical Director by Victor J. Hassid, MD, CPE, FACS, can be found following the references for this article.
Lengthy appointment wait times may adversely impact patient satisfaction,(1–3) patient expectations,(4,5) access to care,(6,7) patient safety,(8) and reputation of health systems.(9) Patients’ expectations for convenience, availability, and service are rising.(10–12) Lengthy wait times for appointments reflect organizational barriers as well as capacity challenges.(13)
Research has demonstrated a positive association between physician leadership and organizational performance as evidenced by improvements in quality and clinical outcomes.(14–17) Despite evidence of the potential benefits of physician leadership, health systems have not historically appointed physicians to leadership roles dedicated to patient access in the ambulatory setting. There is little guidance on how to define this role.
To address this gap of knowledge, this study aimed to create an evidence- and expertise-informed framework to identify elements of the emerging clinician leadership role in ambulatory access in U.S. health systems and to identify the prevalence of clinician leaders assigned to the leadership role in ambulatory access in U.S. health systems. The research findings may benefit health systems considering a leadership role for a clinician to improve access in the ambulatory enterprise.
Methods
The researchers used a convergent mixed-method approach employing interviews and questionnaires to fulfill the research goal. The data are collected concurrently, results are analyzed separately, and the findings are combined. The quantitative results enable generalization, and the qualitative findings incorporate contextual factors by capturing perspectives.(18) The design leverages the strengths of quantitative and qualitative research approaches to investigate and produce a more nuanced understanding of a complex contemporary issue.(18,19)
Interviews followed a semi-structured interview protocol that included questions about the role, competencies, traits, and resource needs as informed by the Alliance for Clinical Education’s framework to describe the essential inputs for the leadership role.(20) The qualitative study was vital to understand the perception of leaders who perform the role. The design of the qualitative portion of the study was guided by the consolidated criteria for reporting qualitative research (COREQ).(21)
Qualitative analyses were conducted by studying transcripts from interviews and were based on a survey of health systems regarding the current and future existence of the role. Two survey rounds were conducted: July–September 2022 and July–August 2023.
The qualitative and quantitative data (first round) were collected concurrently, and the results were integrated.(22) The second round of the quantitative data was conducted 12 months later to examine the change in the existence of the role over time.
Participants
Participants were recruited through the Patient Access Collaborative (PAC) between April and June 2022 (qualitative) and July and September 2022 (quantitative). A purposive sampling technique was used for the qualitative study.(23) Participants were identified through their engagement with educational programs for medical directors offered by the PAC. Twelve experienced physicians and advanced practice providers who functioned as the access medical directors of their health system were invited to participate; 10 accepted the invitation.
For the quantitative study, the survey was sent to the main contacts for each health system that is an organizational member of the PAC. The main contact is the position of a director (or above) in the ambulatory enterprise of the health system they represent.
The PAC consists of U.S. health systems that are academic medical centers, children’s hospitals, and cancer centers. Table 1 shows the geographical regions represented by the PAC. Ninety representatives were invited to participate; 53 accepted. Twelve months later, the 53 participants were surveyed again; 50 agreed to participate. Three of the 50 responses were provided by a new person in the role because the original participant had departed the position. To determine the replacement, the main contact for the PAC was queried; all three replacements agreed to participate. Table 2 displays the characteristics of the quantitative survey participants.


Data Collection
Data were collected for the qualitative and quantitative studies. For the qualitative study, the primary author developed a semi-structured interview guide that was tested at a pilot interview. Interviews were conducted virtually between April and June 2022 using the Zoom technology platform and were recorded with participant permission. The interviews lasted 30 minutes and were transcribed verbatim. Sample questions were:
What, if any, protected time do you have for this role?
How would you describe your leadership characteristics?
What impact would you say that you have had so far on patient access for your organization while in this role?
What message would you give to other health systems that are considering investing in a role like yours?
What training have you had to prepare you for this role?
Concurrently, the authors developed a survey instrument to gather quantitative data on the role of access medical director. For the quantitative study, an electronic survey was distributed using the Survey Monkey® technology platform. Surveys were transmitted three times in 2022 for the first round (July 25, August 2, and September 13) and three times in 2023 for the second round (July 3, July 20, and August 9).
Data Analysis
Transcripts were coded in MAXQDA. The researchers iteratively developed a codebook. Transcripts were analyzed using open coding and tracking issues and themes related to the role, competencies, traits, and resource needs by two independent coders using thematic analysis, a qualitative method used for identifying, analyzing, and reporting patterns (themes) within data.(24–26) The analysis incorporated five steps:
1. To develop an overall impression of the material, the authors read the interviews through several times. Reading the transcripts yielded several themes, identified based on frequency: the importance of collaboration and systems-thinking; the required technical proficiency in data and qualitative skills; centering the efforts on the patient; and the challenges of the time allocated to the role.
2. All transcribed interviews were individually searched for themes, which were then discussed. The themes were divided into codes.
3. The text was coded using the software.
4. The material was synthesized.
5. The final themes were confirmed via consensus to represent the most salient perspectives of the participants.
For the quantitative research, the survey was distributed via email. An analysis of the questionnaire research data demonstrates that 96 participants were sent the survey in July 2022; 53 agreed to participate, representing a 55.2% response rate. For the second survey, which was initiated in July 2023, the 53 participating health system directors were surveyed again, with 50 agreeing to participate, representing a response rate of 94.3%. The data were extracted from the survey instrument and analyzed.
Results
Role. Though there were variations in the job titles of the interviewees, all access medical directors were responsible for an aspect of ambulatory access in their respective health systems. The scope of the role spanned from supporting the contact center that served the ambulatory enterprise to establishing the strategic direction of the health system. The profile of access medical directors who were interviewed is displayed in Table 3.

Participant Characteristics. Ninety health systems were invited to participate in the quantitative survey; 53 accepted in 2022 and 50 in 2023.
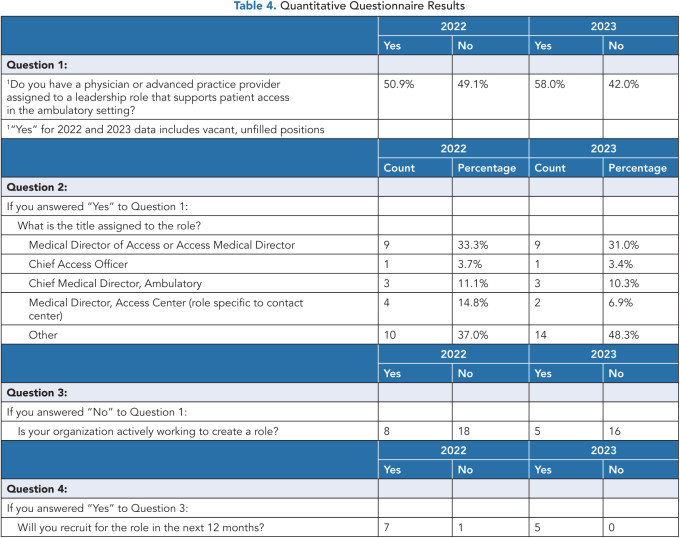
Prevalence of Position. Of the 53 responding health systems, 50.9% indicated that they have a clinician in a leadership role that supports patient access in the ambulatory setting as designated by the health system. One year later, 58.0% of participants reported having a clinician in an access leadership role. This represents an increase of 13.9% from 2022.
Additionally, eight participants in 2022 and five participants in 2023 that did not have a clinician leader tasked with patient access reported being in active development for the role. Seven responding health systems in 2022 and five in 2023 communicated that the role would be established within 12 months.
The most cited titles for the position are medical director of access or access medical director; however, participants reported a variety of position titles (see Table 4).
Discussion
To the best of our knowledge, this is the first study of the clinician leadership role in ambulatory access. Data collection was performed from a semi-structured interview guide of 10 experienced physicians and advanced practice providers who serve in relevant leadership roles. Quantitative data regarding the prevalence of the role were gathered from the leaders of 53 health systems.
Through an assessment of the qualitative data, four key elements were identified regarding the clinician leadership role in ambulatory access: the importance of collaboration and systems-thinking; the required technical proficiency in data and qualitative skills, with inadequate training opportunities at present; the focus on efforts on the patient; and the challenges of the time allocated to the role. The quantitative data revealed that the role of access medical director is present and increasing.
Collaboration and Systems-Thinking. Effective clinician leaders engage in collaborative, team-based models.(27–32) Access in the ambulatory setting represents an opportunity that impacts a multitude of employees, core technological systems, and myriad workflows, necessitating the resources of a team to tackle challenges.
“You can’t be the analyst, the project manager, the physician leader. [You] can’t do [it] all. … You need to make sure you’re partnered correctly with the right team for resources.”
“I don’t do a lot of this work [myself]. I’ve got to have excellent people with me. And so, it’s really [about] team building.”
Emotional intelligence is important in leading teams.(33,34) Relationship development is a foundational element of emotional intelligence.(35,36) Leading the improvement initiatives in access for a health system requires understanding the needs and perspectives of stakeholders.
“…[I]mportant for a medical director … to give themselves time to build relationships and never walk into a meeting saying: ‘Oh, this is how we’re going to do it.’ Just listen. Understand who’s on the other side of that table and what’s their perspective. And that’s how you gain some success.”
“…[A]s a physician…you’re always asked to answer every question, make every decision, and really, you shouldn’t be in this [leadership position]. You need to be standing back and letting other people talk and… show themselves… those individuals…really helping us move along.”
The clinician leader of access is typically partnered with an administrative leader, forming a dyad. Clinician/administrator dyads are growing in health systems, although the literature is limited regarding their impact.(37) The importance of cohesion and synergy in the dyad relationship is vital.(38,39)
“[The dyad is] a relationship that is powerful, has incredibly good results, combines expertise from two different worlds. [However], if you do not invest in that relationship, it can have detrimental effects because then you have a lack of coordination in the sharing of messages, and completely dysfunctional leading of teams moving forward.”
Collaboration is an essential element of leading access improvements in a health system. The system complexity requires clinician leaders to have a high level of emotional intelligence, working in concert with an administrative leader to achieve efficacy.
Possessing a system-level view is considered an essential requirement for leaders to manage problems within complex healthcare organizations.(40–42) Ambulatory practices feature interactive work-system components that may be challenged by barriers related to system-level elements such as the order-entry process.(43) These organizational issues require a macroscopic perspective for interventions to be successful in improving access.
“If you’re a physician, you’re usually in a department, but you have to rise above it, you have to be seen as someone who cares just as much about the faculty [of other specialties], their scheduling outcomes, their ability to see patients, their ability to make their salaries; you have to be able to say to the leaders of those areas … ‘in this role, I’m responsible for serving you.’ ”
Clinician leaders, however, expressed the importance of being familiar with the micro-level workflows. Having a systems-level perspective, while still identifying with the individual clinician, provided an environment for success.
“If that physician [leader] is just a figurehead position, and they don’t really know what’s going on, it’s clear.”
“[B]ecause I live it in clinic myself, I understand the barriers, I understand the pain of having a patient added on and double booked, I understand not having all the records, but what…can [we] do to build infrastructures for our providers…that gives an opportunity for providers to express those pain points - and then…build the solutions as quickly as possible so that we all stay focused on the main thing… taking care of our patients.”
A systems-level approach, complemented by a personal identification, is important for access medical directors to perform their duties and communicate with colleagues.
Technical Proficiency. Beyond medical education and training, clinician leaders may not receive technical skills to support their assigned roles in health systems.(44) Clinician leaders in access expressed frustration regarding limited opportunities to gain skills and competencies in the nascent field. Training was not abundantly available.
“Any time that I signed up for anything, I would [ask]; please, can I get more training?”
Training for technical skills was limited; however, leaders expressed the importance of data capture, handling, and analysis in working on access improvements.
“We deal with tons of data in access. [O]ftentimes, physicians come up with different questions. [It’s important to] to analyze data and be inquisitive…and very detail oriented.”
Data management was cited as a technical skill; however, competency in the leadership domain of change management was vital. Monitoring efficacy, however, was challenging.
“…[W]e are used to tracking KPIs, numbers, graphs with trend, [but] the work that happens for cultural change cannot be tracked that way.”
Clinician leaders acknowledged the importance of proficiency in fostering an environment of psychological safety as an antecedent to quality improvement in access.(45,46)
“How do we establish in such a large organization, an environment of psychological safety for those things to be consistently reported, and for us to be able to assess, learn, study and move into corrective action plans?”
An open-minded, self-reflective attitude was reported as a crucial competency for access medical directors.(47)
“I continuously challenge myself to think of things differently [so I] can become better and serve better the people that I’m supposed to be serving.”
Proficiency in technical skills such as data management was a desired intervention; however, clinician leaders, given the dearth of training opportunities, relied heavily on qualitative skills. Clinician leaders reported exercising abilities associated with psychological safety and change management, skills important for leading today’s complex healthcare organization.(48–50)
Patient-Centeredness. Focusing on the patient is the foundation of an effective healthcare leader.(51,52) Barriers and facilitators to access in ambulatory access are difficult to identify because the entry is initiated by the patient. If the patient does not obtain access, there is no means to identify the root cause of the problem because there is no communication with patients for whom access fails. Therefore, defining the problem, which is a precursor to successful performance improvement,(53,54) is difficult for access medical directors.
“I’m still struggling to decide … exactly how we’re going to measure access. We know we need to work on it, but we can’t prove what’s wrong, or prove that we fixed it.”
Despite the unknown, access medical directors are passionate about helping patients.
“I love taking care of my individual patients in my office, but [to] change the way … that patient care is delivered. I absolutely love this role. … It’s the opportunity to really make change and help patients on a whole different level.”
Access medical directors prioritize their relationships with patients both individually and organizationally. In turn, this characteristic improves the leader’s ability to motivate their peers.
Time Allocation. Role ambiguity, competing demands, and a lack of time and support are perceived as barriers for clinician leaders.(55,56) The role of access medical director is novel, which adds to the challenges of the persons selected for the role.
“[I]t’s…lonely… a lot of people don’t understand all the things that you’re doing. They may not really like something that you suggested or that you’re working on. Or, they may feel that they should be able to get to make [the] decisions, and they don’t understand how much work you’ve put into allowing other people to give their input and that you have such a greater picture of what’s going on.”
Clinician leaders assigned to improve access expressed the view that the time allocated for the emerging role is challenging for them to be effective.
“You wear so many different hats, right? So, I’m still publishing, I’m still giving lectures, I’m still seeing patients. So, it all competes for my time.”
“…It seems sort of ironic that to cut back my access to be able to work on access…it’s been hard to juggle the time for me.”
Access medical directors are not assigned the role on a full-time basis; the protected time varied from 0% to more than 50%. The time allocated to the role is generally considered insufficient.
“So, one day a week. But that’s not enough to actually do it. [W]ishing I had more time to work on it so I could be more effective.”
“…you’re just going to get what you pay for. If you’re only going to give someone 10%, you’re only going to get 10% of their time, don’t expect more.”
Clinician leaders reported personal challenges in time management related to the role. The perception of stakeholders was also notable. If the role is not adequately resourced, that investment is reflective of the importance assigned to achieving the underlying outcome: improving access to ambulatory care.
“The recognition that this role is sufficiently important enough that we’re going to give you the time to actually accomplish it, versus just add it to the rest of what you have to do…sends a message in and of itself.”
The allocation of time is an important consideration for health systems considering the role, according to the access medical directors’ responses.
Adoption. Health systems are investing in the role of access medical director. The responsibilities may be limited to supporting the access center (which is responsible for booking ambulatory appointments) or advising the strategic direction of the organization through guidance about building clinical capacity and managing demand. Comments provided by participants during the quantitative survey elucidated the implementation and growth of the access medical director position:
“The Medical Director role is absolutely critical to the success of access-related initiatives.”
“Our Access Innovations Medical Director is invaluable to physician buy-in, support and ongoing collaboration into access improvement initiatives.”
“It’s a crucial role and the involvement of the medical leadership helps greatly with access efforts.”
“This role is absolutely critical as we are a physician-led organization. Without the Medical Director, we would struggle to make any headway on necessary improvements to patient access.”
“Our Medical Director of Access is invaluable to the team and organization, [they have] been pivotal in developing relationships across primary and specialty care units in accelerating our [a]ccess [s]trategic plan and initiatives.”
The access medical director is emerging as a prominent role in U.S. health systems interested in furthering improvements in ambulatory access.
Limitations
The qualitative research consisted of a small sample of 10 surveys. The relevant domain of patient access in the ambulatory enterprise is narrow, which allowed for thematic saturation with a small sample because of non-probabilistic sampling(57) and salience.(58) The research was guided by the tenants of “information power.”(59)
The participants in the quantitative survey represented academic health systems, children’s hospitals, and cancer centers in the United States; the ambulatory clinics associated with these healthcare organizations are large and complex. Gathering data from leaders and directors who represented these large, complex health systems may limit generalizability of the results. Additional observations and recommendations are suggested.
Conclusion
The study investigated the emerging role of the access medical director in U.S. health systems. A mixed method research approach involving interviews and questionnaire surveys with health systems was adopted for the study. To date, little or no study has been performed about the prevalence and role of the access medical director. This study provides empirical evidence about an emerging leadership role in health systems. By identifying the elements of the role during this nascent stage of the position, the research may serve as a source of reference material for health systems considering the role of access medical director.
Author contributions: Conceptualization, EW; methodology, EW; formal analysis, EW and CP; writing—original draft preparation, EW; writing—review and editing, EW and CP. All authors have read and agreed to the published version of the manuscript.
Acknowledgment: The authors thank Ethan Dubin, MPH, for valuable assistance in coding the transcripts.
References
Habibi MRM, Abadi FM, Tabesh H, Vakili-Arki H, Abu-Hanna A, Eslami S. Evaluation of Patient Satisfaction of the Status of Appointment Scheduling Systems in Outpatient Clinics: Identifying Patients’ Needs. J Adv Pharm Technol Res. 2018;9(2):51–55. https://doi.org/10.4103/japtr.JAPTR_134_18
Kerwin KE, Madison J. The Role of the Internet in Improving Healthcare Quality. J Healthc Manag. 2002;47(4):225–236.
Leddy KM, Kaldenberg DO, Becker BW. Timeliness in Ambulatory Care Treatment: An Examination of Patient Satisfaction and Wait Times in Medical Practices and Outpatient Test and Treatment Facilities. J Ambulatory Care Manage. 2003;26(2):138–149.
Glogovac G, Kennedy ME, Weisgerber MR, Kakazu R, Grawe BM. Wait Times in Musculoskeletal Patients: What Contributes to Patient Satisfaction. J Patient Exp. 2020;7(4):549–553. https://doi.org/10.1177/2374373519864828
Marco CA, Bryant M, Landrum B, Drerup B, Weeman M. Refusal of Emergency Medical Care: An Analysis of Patients Who Left Without Being Seen, Eloped, and Left Against Medical Advice. Am J Emerg Med. 2021;40:115–119. https://doi.org/10.1016/j.ajem.2019.158490
Waller J, Jackowska M, Marlow L, Wardle J. Exploring Age Differences in Reasons for Nonattendance for Cervical Screening: a Qualitative Study. BJOG Int J Obstet Gynaecol. 2012;119(1):26–32. https://doi.org/10.1111/j.1471-0528.2011.03030.x
Rabice SR, Schultz C, Muffly TM. Appointment Wait Times in Female Pelvic Medicine and Reconstructive Surgery: A Mystery Caller Study. Urogynecology. 2021;27(11):681–685. https://doi.org/10.1097/SPV.0000000000001039
Murray M, Berwick DM. Advanced Access Reducing Waiting and Delays in Primary Care. JAMA. 2003;289(8):1035–1040. https://doi.org/10.1001/jama.289.8.1035
Institute of Medicine. Transforming Health Care Scheduling and Access: Getting to Now. Kaplan G, Lopez MH, McGinnis JM, eds. Published online 2015. https://doi.org/10.17226/20220
Comunale MJ, Dermody TS, Peters M, Rudolph JA, Sevco M, Young S. Consumer-Centric Approach to Enhance Access to Pediatric Specialty Care. Am J Manag Care. 2022;28(6):e228–e231. https://doi.org/10.37765/ajmc.2022.89161
Berry LL, Beckham D, Dettman A, Mead R. Toward a Strategy of Patient-Centered Access to Primary Care. Mayo Clin Proc. 2014;89(10):1406–1415. https://doi.org/10.1016/j.mayocp.2014.06.011
Tuzovic S, Kuppelwieser V. Developing a Framework of Service Convenience in Health Care: An Exploratory Study for a Primary Care Provider. Health Mark Q. 2016;33(2):127–148. https://doi.org/10.1080/07359683.2016.1166840
Kreindler SA. Watching Your Wait: Evidence-Informed Strategies for Reducing Health Care Wait Times. Qual Manag Healthc. 2008;17(2):128–135. https://doi.org/10.1097/01.QMH.0000316990.48673.9f
Goodall AH. Physician-leaders and Hospital Performance: Is There an Association? Soc Sci Med. 2011;73(4):535–539. https://doi.org/10.1016/j.socscimed.2011.06.025
Quince T, Abbas M, Murugesu S, et al. Leadership and Management in the Undergraduate Medical Curriculum: a Qualitative Study of Students’ Attitudes and Opinions at One UK Medical School. BMJ Open. 2014;4(6):e005353. https://doi.org/10.1136/bmjopen-2014-005353
Veronesi G, Kirkpatrick I, Vallascas F. Clinicians on the Board: What Difference Does It Make? Soc Sci Med. 2013;77:147–155. https://doi.org/10.1016/j.socscimed.2012.11.019
Lega F, Prenestini A, Spurgeon P. Is Management Essential to Improving the Performance and Sustainability of Health Care Systems and Organizations? A Systematic Review and a Roadmap for Future Studies. Value Health. 2013;16(1, Supplement):S46–S51. https://doi.org/10.1016/j.jval.2012.10.004
Johnson RB, Onwuegbuzie AJ. Mixed Methods Research: A Research Paradigm Whose Time Has Come. Educ Res. 2004;33(7):14–26. https://doi.org/10.3102/0013189X033007014
Fetters MD, Curry LA, Creswell JW. Achieving Integration in Mixed Methods Designs—Principles and Practices. Health Serv Res. 2013;48(6pt2):2134–2156. https://doi.org/10.1111/1475-6773.12117
Morgenstern BZ, Roman BJB, DeWaay D, et al. Expectations of and for Clerkship Directors 2.0: A Collaborative Statement from the Alliance for Clinical Education. Teach Learn Med. 2021;33(4):343–354. https://doi.org/10.1080/10401334.2021.1929997
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. https://doi.org/10.1093/intqhc/mzm042
Creswell JW. A Concise Introduction to Mixed Methods Research. SAGE Publications; 2014.
Robinson RS. Purposive Sampling. In: Michalos, A.C. (eds) Encyclopedia of Quality of Life and Well-Being Research. Springer Dordr. Published online 2014. https://doi.org/https://doi.org/10.1007/978-94-007-0753-5_2337
Braun V, Clarke V. Using Thematic Analysis in Psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa
Scharf J, Vu-Eickmann P, Angerer P, Müller A, in der Schmitten J, Loerbroks A. Work-Related Intervention Needs of Medical Assistants and How to Potentially Address Them according to Supervising General Practitioners: A Qualitative Study. Int J Environ Res Public Health. 2022;19(3):1359. https://doi.org/10.3390/ijerph19031359
Höppchen I, Ullrich C, Wensing M, Poss-Doering R, Suda AJ. Safety Culture in Orthopedics and Trauma Surgery: A Qualitative Study of the Physicians’ Perspective. Unfallchirurg. 2021;124(6):481–488. https://doi.org/10.1007/s00113-020-00917-0
Oostra RD. Physician Leadership: A Central Strategy to Transforming Healthcare. Front Health Serv Manage. 2016;32(3):15–26.
Torti JMI, Inayat H, Inayat A, Lingard L, Haddara W, Sultan N. Perspectives on Physician Leadership: The Role of Character-based Leadership in Medicine. Med Educ. 2022;56(12):1184–1193. https://doi.org/10.1111/medu.14875
Sonnenberg LK, Pritchard-Wiart L, Busari J. The Resident Physician as Leader within the Healthcare team: An Exploratory Inquiry into the Perspectives of Interprofessional Clinicians. Leadersh Health Serv. 2018;31(2):167–182. https://doi.org/10.1108/LHS-08-2017-0046
van Diggele C, Burgess A, Roberts C, Mellis C. Leadership in Healthcare Education. BMC Med Educ. 2020;20(2):456. https://doi.org/10.1186/s12909-020-02288-x
Dine CJ, Kahn JM, Abella BS, Asch DA, Shea JA. Key Elements of Clinical Physician Leadership at an Academic Medical Center. J Grad Med Educ. 2011;3(1):31–36. https://doi.org/10.4300/JGME-D-10-00017.1
van de Riet MCP, Berghout MA, Buljac-Samardžić M, Exel J van, Hilders CGJM. What Makes an Ideal Hospital-based Medical Leader? Three Views of Healthcare Professionals and Managers: A Case Study. PLOS ONE. 2019;14(6):e0218095. https://doi.org/10.1371/journal.pone.0218095
Mansel B. Emotional Intelligence Is Essential to Leadership. Nurs Stand. 2017;31(21):29. https://doi.org/10.7748/ns.31.21.29.s28 . PMID: 28098012
Shrivastava S, Martinez J, Coletti DJ, Fornari A. Interprofessional Leadership Development: Role of Emotional Intelligence and Communication Skills Training. MedEdPORTAL. 2022;18:11247. https://doi.org/10.15766/mep_2374-8265.11247
Lambert S. Role of Emotional Intelligence in Effective Nurse Leadership. Nurs Stand. 2021;36(12):45–49. https://doi.org/10.7748/ns.2021.e11782
Ward HB. Resident Leadership in the Era of COVID-19: Harnessing Emotional Intelligence. Acad Med. 2020;95(10):1521–1523. https://doi.org/10.1097/ACM.0000000000003558
Clouser JM, Vundi NL, Cowley AM, et al. Evaluating the Clinical Dyad Leadership Model: A Narrative Review. J Health Organ Manag. 2020;34(7):725–741. https://doi.org/10.1108/JHOM-06-2020-0212
Saxena A, Davies M, Philippon D. Structure of Health-care Dyad Leadership: An Organization’s Experience. Leadersh Health Serv. 2018;31(2):238–253. https://doi.org/10.1108/LHS-12-2017-0076
American Hospital Association. A Model for Clinical Partnering: How Nurse and Physician Executives Use Synergy as Strategy. Published 2018. Accessed August 22, 2023. https://www.aha.org/system/files/2018-08/plf-issue-brief-clinical-partnering.pdf
Martínez-García M, Hernández-Lemus E. Health Systems as Complex Systems. Am J Oper Res. 2013;3:113–126. https://doi.org/10.4236/ajor.2013.31A011
Lipsitz LA. Understanding Health Care as a Complex System: The Foundation for Unintended Consequences. JAMA. 2012;308(3):243–244. https://doi.org/10.1001/jama.2012.7551
Emami M, Haghdoost AA, Yazdi-Feyzabadi V, Mehrolhassani MH. Identification of Key Components in Health System Using System Thinking Approach: A Scoping Review. Med J Islam Repub Iran. 2023;37:47. https://doi.org/10.47176/mjiri.37.47
Lafferty M, Manojlovich M, Griggs JJ, Wright N, Harrod M, Friese CR. Clinicians Report Barriers and Facilitators to High-Quality Ambulatory Oncology Care. Cancer Nurs. 2021;44(5):E303–E310. https://doi.org/10.1097/NCC.0000000000000832
Brommeyer M, Liang Z. A Systematic Approach in Developing Management Workforce Readiness for Digital Health Transformation in Healthcare. Int J Environ Res Public Health. 2022;19(21):13843. https://doi.org/10.3390/ijerph192113843
Murray JS, Kelly S, Hanover C. Promoting Psychological Safety in Healthcare Organizations. Mil Med. 2022;187(7-8):808–810. https://doi.org/10.1093/milmed/usac041
Aranzamendez G, James D, Toms R. Finding Antecedents of Psychological Safety: A Step Toward Quality Improvement. Nurs Forum (Auckl). 2015;50(3):171–178. https://doi.org/10.1111/nuf.12084
DeMarree KG, Chang YH, Lee T, Venezia A. Listening and Attitude Change. Curr Opin Psychol. 2023;53:101641. https://doi.org/10.1016/j.copsyc.2023.101641
Karimi E, Sohrabi Z, Aalaa M. Change Management in Medical Contexts, Especially in Medical Education: A Systematized Review. J Adv Med Educ Prof. 2022;10(4):219–227. https://doi.org/10.30476/JAMP.2022.96519.1704
Basu K. Change Management and Leadership: An Overview of the Healthcare Industry. In: Health Care Delivery and Clinical Science: Concepts, Methodologies, Tools, and Applications. IGI Global; 2018:85-103. https://doi.org/10.4018/978-1-5225–3926-1.ch005
Beasley L, Grace S, Horstmanshof L. Responding and Adapting to Change: An Allied Health Perspective. Leadersh Health Serv. 2020;33(4):339–349. https://doi.org/10.1108/LHS-07-2019-0050
Hargett CW, Doty JP, Hauck JN, et al. Developing a Model for Effective Leadership in Healthcare: A Concept Mapping Approach. J Healthc Leadersh. 2017;9:69–78. https://doi.org/10.2147/JHL.S141664
Bokhour BG, Fix GM, Mueller NM, et al. How Can Healthcare Organizations Implement Patient-centered Care? Examining a Large-scale Cultural Transformation. BMC Health Serv Res. 2018;18(1):168. https://doi.org/10.1186/s12913-018-2949-5
Ahmed S. Integrating DMAIC approach of Lean Six Sigma and Theory of Constraints Toward Quality Improvement in Healthcare. Rev Environ Health. 2019;34(4):427–434. https://doi.org/10.1515/reveh-2019-0003
Godley M, Jenkins JB. Decreasing Wait Times and Increasing Patient Satisfaction: A Lean Six Sigma Approach. J Nurs Care Qual. 2019;34(1):61–65. https://doi.org/10.1097/NCQ.0000000000000332
Berghout MA, Fabbricotti IN, Buljac-Samardžić M, Hilders CGJM. Medical Leaders or Masters?—A Systematic Review of Medical Leadership in Hospital Settings. PLOS ONE. 2017;12(9):e0184522. https://doi.org/10.1371/journal.pone.0184522
Wiedman C. Navigating Role Conflict: One Professional’s Journey as a New Clinician Leader. BMJ Lead. Published online June 20, 2023:leader. https://doi.org/10.1136/leader-2022-000715
Guest G, Bunce A, Johnson L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods. 2006;18(1):59–82. https://doi.org/10.1177/1525822X05279903
Weller SC, Vickers B, Bernard HR, et al. Open-ended Interview Questions and Saturation. PLOS ONE. 2018;13(6):e0198606. https://doi.org/10.1371/journal.pone.0198606
Malterud K, Siersma VD, Guassora AD. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual Health Res. 2016;26(13):1753–1760. https://doi.org/10.1177/1049732315617444
EXPERT PERSPECTIVE
The Case for Patient Access Medical Director
Victor J. Hassid, MD, CPE, FACS
Woodcock’s and Profeta’s work on the role of medical director in patient access teams comes at a critical moment — amid increasing awareness of the multiple challenges surrounding the very early phases of patients’ care journey and the absolute need for stakeholders and teams to work collaboratively to identify opportunities and provide answers and solutions to the long-standing obstacles and inefficiencies that are compromising patients’ ability to access the appropriate providers at the right time.
I was privileged to be included in the cohort of 10 medical directors for access capacity who were interviewed as part of this study. Along with another 53 access leaders, we were asked qualitative and quantitative questions to analyze the medical director’s role in access operations across multiple healthcare systems in the United States.
Drawing Conclusions
We can extract several conclusions from the study and the survey responses.
First, the role of medical director in patient access operations is undeniably emerging. The number of healthcare organizations that already have an individual serving in this capacity, as well as those that, during the time period of the study, recruited such individuals or were actively developing the role, indicates the increased awareness of the critical nature of the access medical director.
Woodcock’s and Profeta’s research also helps us better understand the knowledge, skills, abilities, and competencies required for clinical leaders in access operations to best serve their patients, teams, and institutions. The researchers also clarify some of the challenges and opportunities the healthcare industry must consider as the understanding of role complexity increases in the years ahead.
The authors highlight the importance of a collaborative mindset and the ability to form genuine partnerships with various stakeholders. This collaboration enhances systems thinking and promotes consideration of diverse perspectives.
Moreover, the importance of dyad leadership models, where a clinical team member partners with an administrator to promote multiple change management initiatives around patient access, is also underscored by some of the answers given by clinical leaders. The dyad members’ different backgrounds, experiences, and training further support an institution’s approach to access challenges.
Furthermore, it’s becoming clear that proficiency in data analytics is an important qualification for the role of access medical director and a consideration when recruiting for this role.
Opportunities for All
This work emphasizes three opportunities that should be considered by all healthcare systems that already have a medical director as part of their team and those currently strategizing about such recruitment. Those opportunities are:
Incorporation of a medical leader in patient access operations if not already in place.
Investment in training opportunities in executive leadership in healthcare and data analytics to allow more meaningful and efficient engagement with teams and data.
Careful planning of appropriate effort and time to allow for greater impact.
The return on the investment of a medical director of patient access, especially those who contribute to the health system’s strategic direction, may not be easy to calculate because not all effects are tangible or measurable. These are, however, the individuals charged to lead by influence as they move the needle in change management initiatives, challenge the status quo, and bring together a variety of groups to address current complex patient access challenges.
Victor J. Hassid, MD, CPE, FACS, is executive medical director of access strategic operations and associate professor of plastic surgery at the University of Texas MD Anderson Cancer Center.

