For as long as I have been involved with the healthcare industry, as a patient and care provider, there has been ongoing commentary on the desperate need to improve healthcare. It seems we are continually declaring that the industry is undergoing transformation and change, always awaiting a new era of better care delivery. Without a doubt, healthcare is the most complex of industries. For an industry based predominantly on the patient–physician relationship, who better to provide expanded leadership and stewardship than the physicians who are its natural and historical leaders? But then, what am I saying here? It is time for change and improvement in healthcare (again)—just like it always is!
Stewardship theory (Figure 1) assumes a humanistic model whereby steward behavior is based on serving others and will, therefore, align with the principal’s interest. Stewardship theorists assume that given a choice between self-serving behavior and pro-organizational behavior, a steward will place a higher value on cooperation than defection. Agency theory (Figure 2), on the other hand, assumes an economic model whereby behavior is based on self-interest and may conflict with the principal’s interest. An agency relationship is created when an organization (the principal) authorizes other people (agents) to act on its behalf. Governance structures that control and monitor agents are prescribed to thwart opportunistic behavior and better align the goals of the principal and agent.
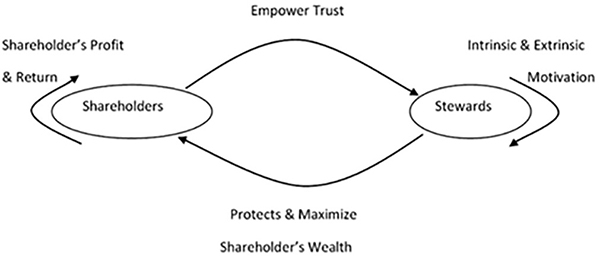
Figure 1. Stewardship theory.
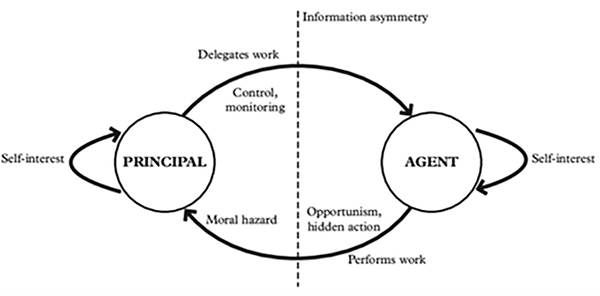
Figure 2. Agency theory.
Professions, generally, are designed to be self-governing and typically monitor the behaviors and outcomes of their licensed practitioners. The medical profession, in particular, has long been viewed by the public as a trusted, honorable profession that does a historically good job of educating, credentialing, monitoring, providing oversight, and self-regulating. Trust and trustworthiness in healthcare have received plenty of attention in the past few years. There was a time not long ago when patients’ trust in physicians was presumed; nowadays, that level of trust and confidence appears to have eroded slightly. However, according to a 2022 Gallup poll, nurses (79%), physicians (62%), and pharmacists (58%) are still the professions most highly trusted by the public.(1)
Perhaps a confluence of our historically based professionalism is now conceptually competing with an inherent need for improved stewardship of our industry and the conflicting behaviors being exhibited throughout the industry related to that of agency theory. There likely are numerous other confounding influences at play as well. As physician leaders, we must continue learning how to better appreciate the genesis of these ever-evolving influences while also learning how to better guide their outcomes.
Paul Keckley, a brilliant healthcare economist, thought leader, and friend of physicians, in a recent posting to the Keckley Report, suggests physicians will indeed play a critical role in shaping the future of healthcare.(2) In his opinion, at minimum, the following issues should be considered:
How value and affordability are defined and actualized in policies and practice;
How the caregiver workforce is developed, composed, and evaluated based on shifting demands;
How incentives should be set and funding sourced and rationalized across all settings and circumstances of service;
How consumerism can be better operationalized;
How prices and costs in every sector (including physician services) can be readily accessible;
How a seamless system of healthcare can be built and refined; and
How physician training and performance can be modernized to participate effectively in the system’s future.
Further considerations, from my perspective, include the following:
American healthcare is a $4 trillion industry and represents nearly 20% of the gross domestic product.
For a family of four, yearly healthcare expenses are now roughly $35,000, and 23% of the population experiences major unexpected medical expenses annually.
In the United States, 23 million people (8.6%) are without health insurance in 2023, and 16% of the overall population has significant medical debt.
Operating losses of U.S. hospitals continue at significant levels, with a third of the top 50 performers being in the red; for the top 500 hospitals, 50% are in the red.
The healthcare industry typically is near the top of all industries in lobbying, spending millions of dollars annually to lobby the federal government—$220 million in 2022 alone.
In the past decade, 540 physicians and more than 2200 hospitals or healthcare companies negotiated to pay the U.S. government more than $26.8 billion in settlements or judgments related to potential criminal activity, according to Reuters.(3)
According to the Physicians Advocacy Institute, nearly 70% of American physicians are now employed in large groups, health systems, or private equity–sponsored systems.(4) The Association of American Medical Colleges regularly reviews the manpower of physicians, and in its most recent report suggests there will be shortages of between 37,800 and 124,000 physicians by 2034.(5) Clearly a shift is occurring, and, separate from the high rates of physician burnout, these shifts need to be followed closely over time.
The Department of Health and Human Services Inspector General recently found that 13% of hospitalized Medicare patients experienced preventable harm during a hospital stay in October 2018.(6) A New England Journal of Medicine study of patients hospitalized in Massachusetts in 2018 showed that 7% had a preventable adverse event, with 1% suffering a preventable injury that was serious, life-threatening, or fatal.(7)
We all readily recognize the various statistics and could spend endless hours debating their worth or cause. Raging against the current state of affairs may serve a purpose on some level, although it typically does not create positive change in resolving issues at hand. Trying to conquer these various influences to bring healthcare systems back to historical practices is nonproductive at this stage of our industry’s evolution. The data already show it is not working.
Physician leadership can be, and in fact is, more than simply detailing data. Physicians are trained to be problem solvers and to provide remedies for ailments. Embracing our professional responsibility as leaders, coupled with a renewed sense of stewardship for the industry, should capably provide the needed path forward. Numerous remedies will be required.
Although I do not have all the answers, in my opinion, learning to collaborate with clinical and nonclinical cohorts in the delivery system is a necessary step forward. Physician leadership needs ways to influence healthcare in the nonclinical sectors of the industry. For example, the UnitedHealth company is now the largest employer of physicians (75,000), and it is placed among the top five Fortune 500 companies. Several other healthcare companies are also listed near the top of that list.
Physician leadership belongs to us all. Let us not waste the opportunity to collaborate more closely for the change warranted in an industry that is so deeply personal for everyone. We, our patients, and our families will all benefit from these efforts.
References
Brenan M. Nurses retain top ethics rating in U.S., but below 2020 high. Gallup.com. January 10, 2023. https://news.gallup.com/poll/467804/nurses-retain-top-ethics-rating-below-2020-high.aspx .
Keckley P. Special Report: Physicians on the brink or at the starting line? The Keckley Report. May 20, 2023. https://paulkeckley.com/the-keckley-report/2023/5/30/special-report-physicians-on-the-brink-or-at-the-starting-line .
Berens M. How doctors buy their way out of trouble. Reuters. May 24, 2023. www.reuters.com/investigates/special-report/usa-healthcare-settlements .
Avalere Health. COVID-19’s impact on acquisitions of physician practices and physician employment 2019-2020. Physicians Advocacy Institute. June 2021. www.physiciansadvocacyinstitute.org/Portals/0/assets/docs/Revised-6-8-21_PAI-Physician-Employment-Study-2021-FINAL.pdf .
The complexities of physician supply and demand: projections from 2019 to 2034. American Association of Medical Colleges. Washington, DC: AAMC; June 2021. www.amc.org/media/54681/download?attachment .
Grimm CA. Adverse Events in Hospitals: A Quarter of Medicare Patients Experienced Harm in October 2018. US Department of Health and Human Services, Office of Inspector General. May 2022. https://oig.hhs.gov/oei/reports/OEI-06-18-00400.pdf .
Bates DW, Levine DM, Salmasian J, et al. The safety of inpatient health care. N Engl J Med. 2023;388:142-153. https://doi.org/10.1056/NEJMsa2206117 .
Excerpted from Inspiring Growth and Leadership in Medical Careers: Transform Healthcare as a Physician Leader (American Association for Physician Leadership, 2024).

